AESA PROGRAMMES
- Building R&D Infrastructure
- Developing Excellence in Leadership, Training and Science in Africa (DELTAS Africa)
- Human Heredity and Health in Africa (H3Africa)
- Africa’s Scientific Priorities (ASP)
- Innovation & Entrepreneurship
- Grand Challenges Africa
- Grand Challenges Innovation Network
- Rising Research Leaders/Post-Docs
- AESA RISE Postdoctoral Fellowship Programme
- African Postdoctoral Training Initiative (APTI)
- Climate Impact Research Capacity and Leadership Enhancement (CIRCLE)
- Climate Research for Development (CR4D)
- Future Leaders – African Independent Research (FLAIR)
- Critical Gaps In Science
- Clinical Trials Community (CTC)
- Community & Public Engagement
- Mobility Schemes: Africa-India Mobility Fund
- Mobility Schemes: Science and Language Mobility Scheme Africa
- Research Management Programme in Africa (ReMPro Africa)
- Science Communication/Africa Science Desk (ASD)
- Financial Governance: Global Grant Community (GGC)
- AAS Open Research
- CARI Programmes
- Evidence Leaders Africa (ELA)

News
Break down barriers to deal with drug resistance
166
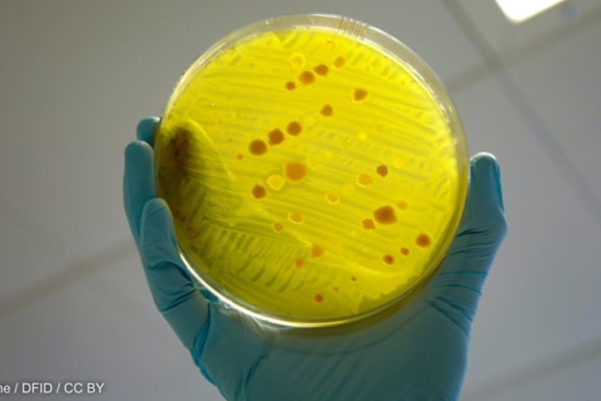
Break down barriers to deal with drug resistance
Professor Olanike Adeyemo, Fellow of the AAS
The COVID-19 pandemic has thrown a spotlight on the growing crisis of antibiotic resistance and the urgent need for global efforts to prevent this challenge from taking root. Much attention has been focused on how humans misuse antibiotics — either because they lack access to appropriate treatment or fail to complete antibiotic treatment due to lack of funds.
But unless we start looking beyond humans and recognize how the use of antibiotics in animals impacts our broader effort to reduce human antibiotic resistance, then we are unlikely to succeed in the long term.
The indiscriminate use of antibiotics for COVID-19 patients could lead to 10 million deaths by 2050, by some counts, if nothing is done about the menace of antimicrobial resistance. Most of the deaths are likely to occur in Asia and Africa. The COVID-19-exacerbated abuse of a wide array of broad-spectrum antibiotics will no doubt promote the spread of resistant microorganisms, especially in developing countries where such drugs are often readily available over-the-counter.
Antimicrobials cover all drugs used to treat bacteria, fungi, protozoa, etc., while antibiotics just act on bacterial agents. Last year’s World Health Organization antimicrobial resistance surveillance report revealed an alarmingly high level of antimicrobial-resistant infections with high levels of resistance to last-resort antibiotics such as carbapenems. These carbapenems are a class of highly effective antibiotic agents commonly used for the treatment of severe or high-risk bacterial infections.