AESA PROGRAMMES
- Building R&D Infrastructure
- Developing Excellence in Leadership, Training and Science in Africa (DELTAS Africa)
- Human Heredity and Health in Africa (H3Africa)
- Africa’s Scientific Priorities (ASP)
- Innovation & Entrepreneurship
- Grand Challenges Africa
- Grand Challenges Innovation Network
- Rising Research Leaders/Post-Docs
- AESA RISE Postdoctoral Fellowship Programme
- African Postdoctoral Training Initiative (APTI)
- Climate Impact Research Capacity and Leadership Enhancement (CIRCLE)
- Climate Research for Development (CR4D)
- Future Leaders – African Independent Research (FLAIR)
- Critical Gaps In Science
- Clinical Trials Community (CTC)
- Community & Public Engagement
- Mobility Schemes: Africa-India Mobility Fund
- Mobility Schemes: Science and Language Mobility Scheme Africa
- Research Management Programme in Africa (ReMPro Africa)
- Science Communication/Africa Science Desk (ASD)
- Financial Governance: Global Grant Community (GGC)
- AAS Open Research
- CARI Programmes
- Evidence Leaders Africa (ELA)

News
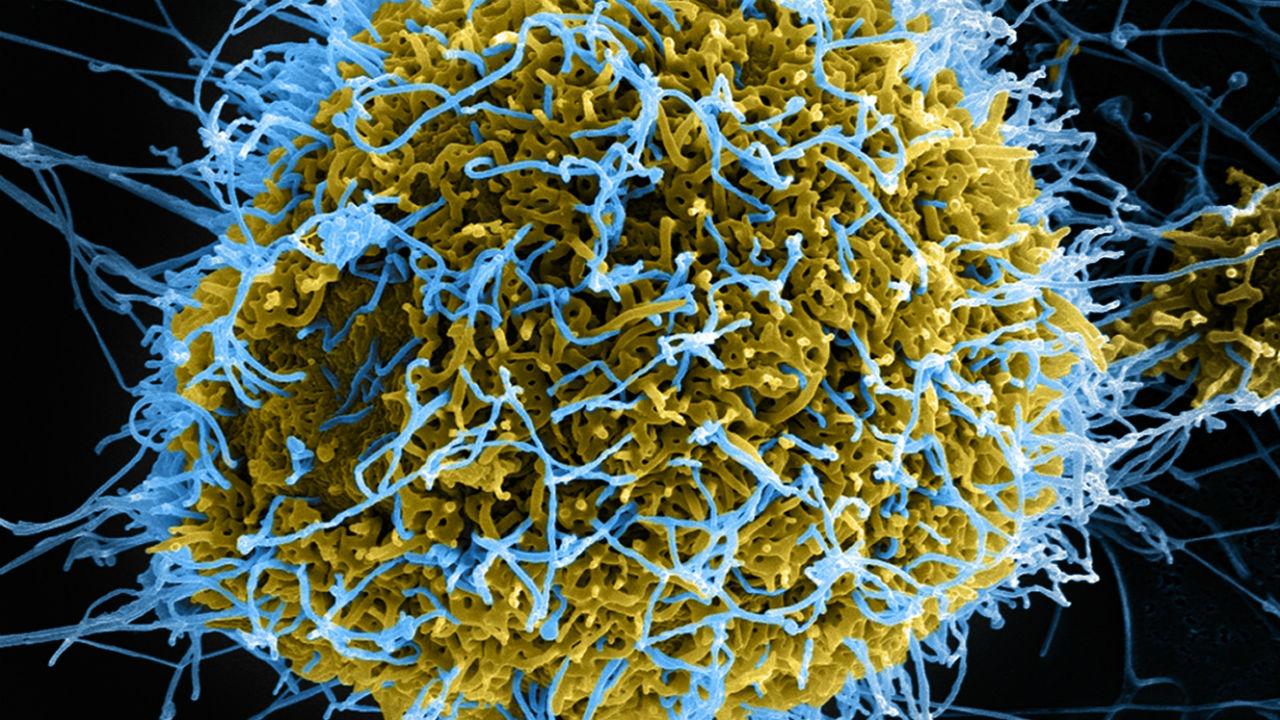
Genomics research in controlling Neglected Tropical Diseases
165
Genomics research in controlling Neglected Tropical Diseases
 Enock Matovu is a molecular biologist and Principal Investigator for the Genetic Determinants of Two Neglected Tropical Diseases (TrypanoGEN+) project under the Human Heredity and Health in Africa (H3 Africa) programme. H3 Africa supports population-based studies that use genetic, clinical and epidemiological tools to better understand how the interplay between human genes and the environment influence disease susceptibility, pathogenesis and prevention, with the goal of improving the health of African populations. H3 Africa is implemented through the AESA Platform. AESA (the Alliance for Accelerating Excellence in Science in Africa) is a funding, agenda-setting, programme management initiative of the African Academy of Sciences (AAS), the African Union Development Agency (AUDA-NEPAD), founding and funding global partners, and through a resolution of the summit of African Union Heads of Governments. H3 Africa is supported by the National Institute of Health (NIH), Wellcome, and African Society of Human Genetics (AfSHG).
Enock Matovu is a molecular biologist and Principal Investigator for the Genetic Determinants of Two Neglected Tropical Diseases (TrypanoGEN+) project under the Human Heredity and Health in Africa (H3 Africa) programme. H3 Africa supports population-based studies that use genetic, clinical and epidemiological tools to better understand how the interplay between human genes and the environment influence disease susceptibility, pathogenesis and prevention, with the goal of improving the health of African populations. H3 Africa is implemented through the AESA Platform. AESA (the Alliance for Accelerating Excellence in Science in Africa) is a funding, agenda-setting, programme management initiative of the African Academy of Sciences (AAS), the African Union Development Agency (AUDA-NEPAD), founding and funding global partners, and through a resolution of the summit of African Union Heads of Governments. H3 Africa is supported by the National Institute of Health (NIH), Wellcome, and African Society of Human Genetics (AfSHG).
Summary
The study reveals that even from a genetic point of view, the different communities across Africa have coped differently to their co-existence with disease causing organisms. This might be due to the different environmental factors in their localities, perhaps including diet. The unprecedented diversity within Africa dictates that each community/ethnicity dataset should be analysed separately in order to accurately identify the genetic predispositions to communicable diseases. Taking this route might lead to effective disease control solutions tailored to specific communities/ethnicities.
Background
Neglected Tropical Diseases (NTDs) are recognized by the World Health Organization (WHO) as a diverse group of communicable diseases that afflict more than a billion of the most economically disadvantaged inhabitants of this planet. They comprise mainly parasitic infections and are typically characterized by long term morbidity. NTDs have a substantial impact on the quality of life of affected communities as measured by the millions of Disability Adjusted Life Years (DALYs) lost to these highly debilitating diseases. These so-called “diseases of poverty” are significantly present in rural Africa. They are associated with complex life cycles and epidemiology, which makes them difficult to combat effectively. Their complex epidemiology may involve various vectors and animal reservoirs (neglected zoonotic diseases); some are soil-transmitted, and others are water-borne, which makes provision of safe water, sanitation and hygiene (WASH) critically important.
TrypanoGEN+ is a consortium/network of countries across Francophone and Anglophone Africa (Cameroon, Democratic Republic of the Congo, Guinea, Ivory Coast, Malawi, South Africa, Uganda) and two countries in the Northern hemisphere, France and the United Kingdom. TrypanoGEN+ is focused on two parasitic NTDs: Human African Trypanosomiasis (HAT), that is caused by trypanosomes (flagellated protozoans) and transmitted by fly bites, and schistosomiasis (Bilharzia), that is transmitted by contact with fresh water bodies infested with snails that act as intermediate hosts for the schistosomes (blood flukes) in the larval stages. The aim of our study is to investigate the role of host and parasite genetics in determining infection outcomes (disease phenotypes).
Our recent study of HAT reveals the presence of trypanosome-infected individuals tolerant of the infection (termed “trypanotolerant”) in whom the progression of disease is delayed from the early stage (when the parasites are confined to blood and lymphatic tissue) to the often lethal late stage, when the parasites cross into the central nervous system to trigger the typical symptoms of sleeping sickness. Inversely, in schistosomiasis, the most interesting disease manifestation is the subset which is hypersensitive, carrying a heavy worm burden and propagating the infection by shedding millions of eggs in the environment, from which new individuals are infected when they come into contact with infested freshwater bodies. Thus, individuals who are likely to play a significant role in disease transmission are, in the case of HAT, asymptomatic cases of trypanosomiasis that go unnoticed and remain as uncontrolled reservoir of infection.
For schistosomiasis, the important group are the hypersensitive individuals who harbour a high blood fluke load and release millions of parasite eggs to contaminate freshwater bodies and sustain transmission. These extreme phenotypes are never targeted for treatment, posing a challenge to the WHO goal of elimination of these NTDs as public health problems. For this reason, our research focus is investigating how the human natural make-up and interactions with the parasites lead to the observed differences in disease manifestations. We also wish to understand if the different disease manifestations impact on onward disease transmission. Thus TrypanoGEN+ seeks to unravel the components of the human body that render certain host tolerant to trypanosomiasis or highly sensitive to Bilharzia. This might provide opportunities to devise alternative approaches to control these diseases more effectively.
Description of the study
We seek to determine the hereditary units of the human body (the genes) that are associated with the different disease traits or manifestations through Genome Wide Association Studies (GWAS), in which we analyse and compare the entire genetic make-up of numerous individuals, both diseased and no-disease. We shall also study these traits within families, using the so-called Family Based Association Studies (FBAT). In our study populations, we shall as well study those genetic markers that were previously implicated in other populations, using the Candidate Gene Association Studies (CGAS) approach. We shall then confirm our findings in laboratory animals experimentally infected with the respective pathogens. In collaboration with national control programs, we have organized field surveys in affected communities to obtain informed consent and include volunteers in the study to be classified according to disease severity. We shall start by looking for any indication of specific immune responses to infection (using antibody tests), followed by demonstration of the parasites in body fluids (HAT) or parasite eggs in stool (schistosomiasis). Consequently, our study cohort represents a well characterized collection of samples from inhabitants of HAT- and schistosomiasis-endemic areas. Samples from these volunteers will be used in experiments to pinpoint genetic makers for HAT tolerance or schistosomiasis hypersensitivity.
Outcomes
Over 4,500 samples were collected across the network from which the genomes of 230 Africans from five countries were sequenced; no previous studies have sequenced samples at this scale. An incidental but important finding was made from the 50 Nilo-Saharan Lugbara people from Northern Uganda that were included in the study: this population is genetically highly divergent from other African populations, revealing an even greater African diversity than had previously been known.
In the course of this study, we also examined the relationship between chronic kidney disease (CKD) and human African trypanosomiasis, an association which had previously been proposed to reveal one of the strongest examples of how a host’s response to a parasite (trypanosomiasis in this case) can lead to selection genes that can make the human vulnerable to another disease (CKD). This relationship centres on modifications of a certain human protein, (APOL1), which protects humans from sleeping sickness by disrupting the trypanosomes, but unfortunately the kidney cell too are disrupted leading to CKD.
In addition to candidate gene studies, we conducted a two-stage GWAS with H3Africa genotyping SNP chip (1115 cases, 1153 controls) to detect more variants in other genes that affect susceptibility to trypanosomiasis. Two genes were identified that were validated in a second round of testing and are the subject of current confirmatory studies using mouse models. From the candidate gene association studies, we have found that different populations have different genetic adaptations to infection, perhaps determined by the different environments where they live. Thus, a genetic marker that protects individuals from trypanosomiasis in Malawi is different to that conferring the same in Guinea for example. Meanwhile, similar work to determine host genetic predisposition to schistosomiasis is still in early discovery phase.
To-date, six PhD and three MSc students have been trained, and there is an additional cohort of nine PhD students, two postdocs who have progressed to permanent research positions and two senior and four junior postdocs moving up the career ladder. All these individuals are considered part of our research team. In addition, research administration, computing and laboratory infrastructure at African? partner institutes (including bio banking facilities) have been set up. These are vital resources to consolidate gains made so far and provide sustainable resources to kick-start future discovery projects.
Moreover, in the course of our fieldwork, we directly contribute to disease control by identifying and referring patients for treatment, thereby reaping immediate benefits from a control point of view.
Lessons learned
Findings to-date indicate that an even greater genetic diversity across the African continent exists than was previously known. The candidate gene association study results indicate that different populations adjust and respond to pathogens by evolving in different ways to cope with the infections with which they have co-existed for generations. Thus, no single gene is likely to be responsible for the disease phenotypes in all the affected populations. For this reason, disease susceptibility markers may be different in the different populations, although pathways may be in common.
We have learned new approaches to genomics research in rural communities affected by these NTDs that are sensitive to the ethical, legal and social issues (ELSI) associated with genomics research. A robust community engagement plan has enabled us to be in constant touch with the communities with whom we work and has improved our ability to communicate results to the lay research audiences in which this cutting-edge genomics research is being conducted.
Potential Impact
If this study confirms genes and/or pathways associated with disease phenotype/outcome, it will open avenues for development of new control tools and strategies. For example, it has the potential to identify novel molecules to be used to design supportive therapy to complement conventional chemotherapy that to this point has only targeted the parasite, with no consideration to aiding the host to fight back. In addition, new tools to screen populations for genetic markers of disease susceptibility can be developed. This could assist national control programs to identify the most vulnerable populations in order to tailor control strategies so that limited resources are prioritized to communities where they are most needed. Moreover, while undertaking our studies, we are building a critical mass of African researchers with expertise in genetics/genomics who will be ongoing contributors to the development of research agendas in research-endemic countries, leading to new control tools and strategies.