AESA PROGRAMMES
- Building R&D Infrastructure
- Developing Excellence in Leadership, Training and Science in Africa (DELTAS Africa)
- Human Heredity and Health in Africa (H3Africa)
- Africa’s Scientific Priorities (ASP)
- Innovation & Entrepreneurship
- Grand Challenges Africa
- Grand Challenges Innovation Network
- Rising Research Leaders/Post-Docs
- AESA RISE Postdoctoral Fellowship Programme
- African Postdoctoral Training Initiative (APTI)
- Climate Impact Research Capacity and Leadership Enhancement (CIRCLE)
- Climate Research for Development (CR4D)
- Future Leaders – African Independent Research (FLAIR)
- Critical Gaps In Science
- Clinical Trials Community (CTC)
- Community & Public Engagement
- Mobility Schemes: Africa-India Mobility Fund
- Mobility Schemes: Science and Language Mobility Scheme Africa
- Research Management Programme in Africa (ReMPro Africa)
- Science Communication/Africa Science Desk (ASD)
- Financial Governance: Global Grant Community (GGC)
- AAS Open Research
- CARI Programmes
- Evidence Leaders Africa (ELA)

News
Identifying tuberculosis treatment gaps in Uganda
216
Identifying tuberculosis treatment gaps in Uganda
Simon Kimuda is a Ugandan post-doctoral research fellow affiliated to the MRC/UVRI and LSHTM Uganda Research Unit and the London School of Hygiene & Tropical Medicine and is currently based at the Francis Crick Institute – UK. MUII-plus (the Makerere University-Uganda Virus Research Institute Infection and Immunity programme) is one of the 11 Developing Excellence, Leadership, and Training in Science in Africa (DELTAS Africa) programmes. DELTAS Africa funds Africa-based scientists to amplify the development of world-class research and scientific leadership on the continent while strengthening African institutions. DELTAS Africa is implemented through the AESA Platform. AESA (The Alliance for Accelerating Excellence in Science in Africa) is a funding, agenda-setting, programme management initiative of the African Academy of Sciences (AAS), the African Union Development Agency (AUDA-NEPAD), founding and funding global partners, and through a resolution of the summit of African Union Heads of Governments. DELTAS Africa is supported by Wellcome and the United Kingdom Foreign, Commonwealth and Development Office (FCDO formerly DFID).
Summary
In this blog, Kimuda discusses the major obstacles to the development of an effective vaccine against tuberculosis (TB). He describes the origin of his interest in the field of biology and how his studies of immunity to TB may provide important insights to the design of new vaccines and treatments for this disease.
An early interest in biology
I have always been curious about life. As a child, I wondered how we lived and breathed and why some people got sick while others did not. My affinity for biology was evident in primary and secondary school. I spent hours going over biology textbooks even when there were no exams to prepare for or assignments to work on. This interest led me to pursue a degree in laboratory biomedical science at the then-Faculty of Veterinary Medicine of Makerere University. My favourite subject was molecular biology -- the study of proteins and nucleic acids such as DNA and their role in maintaining life. I was also introduced to immunology -- the study of the immune system, a subject that I grew to love.
In the third year of my undergraduate studies, I earned a coveted placement in our Faculty’s molecular biology and immunology lab. While there, I had the opportunity to do the kind of research that I had only read about in books. It was a truly exciting time! I studied the genes of trypanosomes, the parasites that cause sleeping sickness. I learned how to use this information to develop vaccines that could be used to evoke immunity against this infection. The experience left me with a deep urge to learn more about immunology and I yearned to find ways that I could apply what I had learned to help fight disease.
I was very fortunate to volunteer at Uganda’s national TB reference laboratory after my undergraduate studies. While there, I gained a deep appreciation of the TB epidemic in the country. I witnessed the pain and suffering of TB patients in the TB wards of Uganda’s national referral hospital, Mulago. I decided to commit the next few years of my life to the study of this disease. I won a scholarship from MUII to do an MSc in Immunology and Clinical Biology and embarked on a career in TB immunology research.
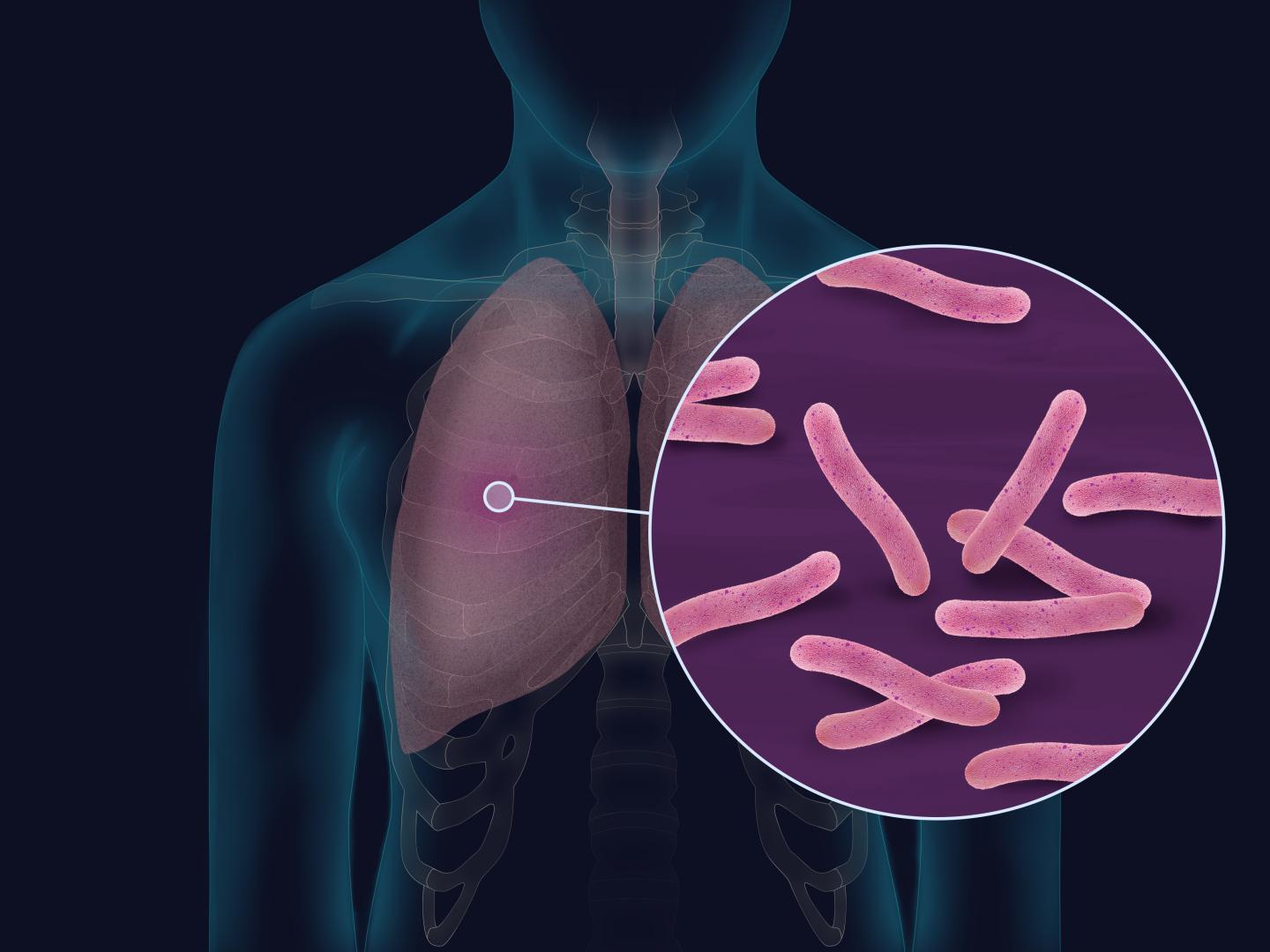
Tuberculosis: the leading cause of death from a single infectious agent
Tuberculosis is an infectious disease that is caused mainly by the bacterium, Mycobacterium tuberculosis (M. tuberculosis). It is the leading cause of death from a single infectious agent, having claimed approximately 1.5 million lives in the year 2018. The disease is of global concern and could easily be called “the other pandemic” in these tumultuous times. TB is primarily a disease of the poor, affecting large areas of the tropics, including sub-Saharan Africa. Although a vaccine against TB exists, it performs poorly in the regions where it is most needed. This vaccine, known as BCG, has markedly reduced efficacy in equatorial regions of the world; researchers are still trying to figure out why this is the case. The BCG vaccine does have the ability to prevent severe forms of TB in young children, but the protection that it offers wanes with age. New and more effective vaccines against TB are urgently needed!
Studying the immune system to discover new vaccines and treatments
The major impediment to the development of new TB vaccines is the lack of an established “correlate of immunological protection”. This is a measure of the immune response that can be used to tell whether or not someone’s body has the ability to effectively fight off TB and remain protected from the disease. One way that we can discover these correlates is by studying populations of people who have been exposed to TB. This can help us identify which elements of the immune response play critical roles in protection; this information can in turn be used to design more effective vaccines. This area of research has been the focus of my graduate studies and post-doctoral research.
Shortly after the completion of my MSc training, I won a competitive PhD fellowship from MUII to study immune responses in people with TB at Makerere University. My project, entitled, “Effects of M. tuberculosis infection on B cell responses” was supervised by Drs. Stephen Cose, John Raynes and Bernard Bagaya. In my second year of training, I was awarded a prestigious Commonwealth Spit-site PhD fellowship that supported a year-long placement at the London School of Hygiene & Tropical Medicine (LSHTM). My main interest was in antibodies, little proteins produced by a compartment of our immune cells known as B cells that fight off disease-causing germs such as bacteria and viruses. I tested the blood of TB sufferers and their close contacts to understand how antibodies change in different states of TB infection in healthy but exposed people. I found that antibodies from TB patients bound more strongly to parts of M. tuberculosis bacteria than those from healthy people, and that these antibodies also bound to a broad range of germs including flu-causing viruses, measles virus and bacterial toxins such as tetanus. The findings left me with more questions than answers! If strongly binding antibodies are produced in people with TB, why aren’t they effective? Why do people with TB have antibodies that bind strongly to different disease-causing germs and how can this be exploited to make new treatments and vaccines?
A long but exciting journey ahead!
Since the completion of my post-graduate studies, MUII leadership has continued to support my efforts to secure follow-on funding to answer these interesting questions. The programme director, Prof. Alison Elliott, continues to mentor me. I won funding from the Immunising Pregnant Women and Infants Network, the MRC/UVRI and LSHTM Uganda Research Unit, and most recently, the Crick African Network, to support my postdoctoral research. I am currently doing work at the Francis Crick Institute and LSHTM – UK to understand the role of antibodies in protection against TB. I study how antibody binding strength affects how well these proteins stop the growth of M. tuberculosis bacteria in test tubes. I am learning new ways to measure how well TB vaccines work in human populations with the aim of transferring these technologies to Uganda. There is still a lot to be done but I look forward to an exciting journey of discovery ahead.