AESA PROGRAMMES
- Building R&D Infrastructure
- Developing Excellence in Leadership, Training and Science in Africa (DELTAS Africa)
- Human Heredity and Health in Africa (H3Africa)
- Africa’s Scientific Priorities (ASP)
- Innovation & Entrepreneurship
- Grand Challenges Africa
- Grand Challenges Innovation Network
- Rising Research Leaders/Post-Docs
- AESA RISE Postdoctoral Fellowship Programme
- African Postdoctoral Training Initiative (APTI)
- Climate Impact Research Capacity and Leadership Enhancement (CIRCLE)
- Climate Research for Development (CR4D)
- Future Leaders – African Independent Research (FLAIR)
- Critical Gaps In Science
- Clinical Trials Community (CTC)
- Community & Public Engagement
- Mobility Schemes: Africa-India Mobility Fund
- Mobility Schemes: Science and Language Mobility Scheme Africa
- Research Management Programme in Africa (ReMPro Africa)
- Science Communication/Africa Science Desk (ASD)
- Financial Governance: Global Grant Community (GGC)
- AAS Open Research
- CARI Programmes
- Evidence Leaders Africa (ELA)

News
Preventing transmission of hepatitis B in Senegal
216
Preventing transmission of hepatitis B in Senegal
Summary
This blog by Fabien Taieb, Head of the clinical research development program at the Epidemiology, Clinical Research and Data Sciences department of Institut Pasteur of Dakar, Senegal, and the Alliance for Accelerating Excellence in Science in Africa (AESA) grantee under Grand Challenges Africa (GC Africa) programme, discusses the prevention of mother-to-child transmission of hepatitis B by improving access to the monitoring of hepatitis B virus in the blood. This approach is synergistic with a birth dose vaccine.
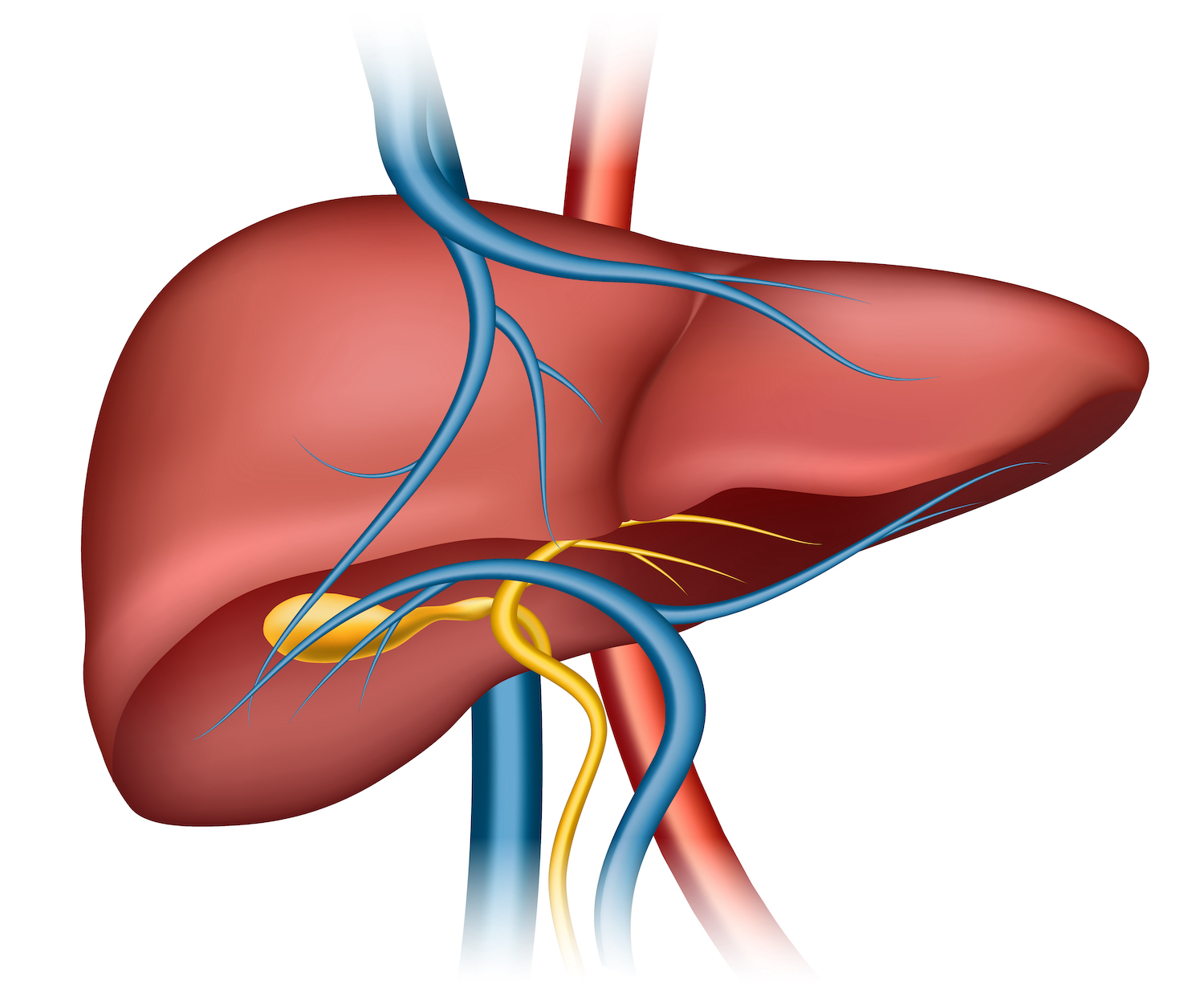
Hepatitis B: A major global public health problem in Africa
Viral hepatitis is the 7th leading cause of death worldwide and kills more people than any other major infectious disease (e.g. HIV, tuberculosis, malaria). About half of all hepatitis deaths are attributable to hepatitis B virus (HBV). Sub-Saharan Africa (SSA) suffers from the highest HBV prevalence in the world (>8%); an estimated 55,000 people die prematurely every year from HBV-related liver disease. Moreover, more than 60% of HBV-related liver diseases are attributable to mother-to-child transmission (MTCT), and 80–90% of infants infected during the first year of life develop chronic infection.
To reduce the disease burden in sub-Saharan Africa, it is imperative to implement effective prevention of new infections via the universal implementation of HBV birth-dose vaccine, full vaccine coverage, access to affordable diagnostics to identify HBV-infected individuals and linkage to care and antiviral treatment.
Fight against HBV mother-to-child transmission
To prevent HBV mother-to-child transmission, the World Health Organization (WHO) recommends the administration of HBV vaccine to all babies within 24 hours of birth. However, this strategy alone is unlikely to be adequate in Africa for two reasons. First, only 10% of African babies receive this vaccine within a day of birth because current practice in many countries is to administer it starting at 6-8 weeks of age using fixed combination vaccines. And even for countries with a policy of administration at birth, the policy is often not implemented because many births take place at home and not in health facilities.
Second, while the birth dose vaccine alone is sufficient to prevent mother-to-child transmission in mothers with low serum HBV DNA, 20-30% of women with high viral load still infect their infants despite timely vaccination. Consequently, in 2020, WHO issued new guidelines for the prevention of mother-to-child transmission of hepatitis B, recommending administration of antiviral therapy during pregnancy in women carrying high HBV DNA levels (>200,000 IU/mL), in addition to the universal birth dose vaccine. Compared to the birth dose vaccine alone, this new strategy may be better adapted to sub-Saharan Africa, because the vast majority (78%) of pregnant women attend at least one antenatal care visit, while only half deliver their baby at health facilities. This suggests that “screen-and-treat” starting with antenatal care may result in wider service coverage than vaccine provided at health facilities immediately after birth. Therefore, detection of HBV infection during pregnancy and measurement of viral load levels are crucial to identify patients who must receive effective treatment in order to prevent the spread of the disease.
However, real-time Polymerase Chain Reaction (PCR), the standard test to quantify HBV DNA levels, is costly and requires trained personnel, making it inaccessible to many patients, especially in decentralized areas of Africa. We, therefore, propose use of the loop-mediated isothermal amplification (LAMP) assay, a simpler and low-cost detection technique, for the population segment with limited access to HBV virological monitoring.
New tool for access to HBV virological monitoring
LAMP has been recommended by WHO to diagnose tuberculosis in low resource settings. However, its use to diagnose high hepatitis B viral loads has not been well studied. Therefore, Dr Jessica Vanhomwegen and Dr Yusuke Shimakawa, colleagues at the Institut Pasteur, Paris, have developed a HBV-LAMP assay to identify people with a high level of viruses in the blood.
We will conduct a field study to validate, the LAMP assay to semi-quantify hepatitis B virus (HBV) DNA level in pregnant women. We will assess the viability for this inexpensive and user-friendly assay to monitor and mitigate mother-to-child transmission of HBV in Senegal, a country with high prevalence of HBV.
About Fabien Taieb
Fabien Taieb is a French clinician, specialising in Infectious Diseases. He heads the clinical research development program at the Epidemiology, Clinical Research and Data Sciences department of Institut Pasteur of Dakar, and is an innovator supported by Grand Challenges Africa (GC Africa). GC Africa promotes Africa-led scientific innovation to help countries achieve the Sustainable Development Goals by awarding grants to Africa’s most promising innovators. It is implemented through the Alliance for Accelerating Excellence in Science in Africa (AESA), a funding, agenda-setting, programme management initiative of the African Academy of Sciences (AAS), the African Union Development Agency (AUDA-NEPAD), founding and funding global partners, and through a resolution of the African Union Heads of Governments. GC Africa is supported by the Bill & Melinda Gates Foundation, Swedish International Development Cooperation Agency (Sida), and the German Federal Ministry of Education and Research (BMBF).